This strategy has been successful with both malaria and HIV. JL
Nicole Wetsman reports in The Verge:
While most research studies focus on treatments for people who are already sick with COVID-19, some researchers are looking to see if they can stop people from getting sick in the first place. Preventive drugs have been used for decades to protect against malaria. There’s no effective vaccine against HIV, but people can take a daily medication that reduces their risk of contracting it by 99%. The medication is a pre-exposure prophylactic, or PrEP — a drug used to prevent disease in people who haven’t yet been exposed.
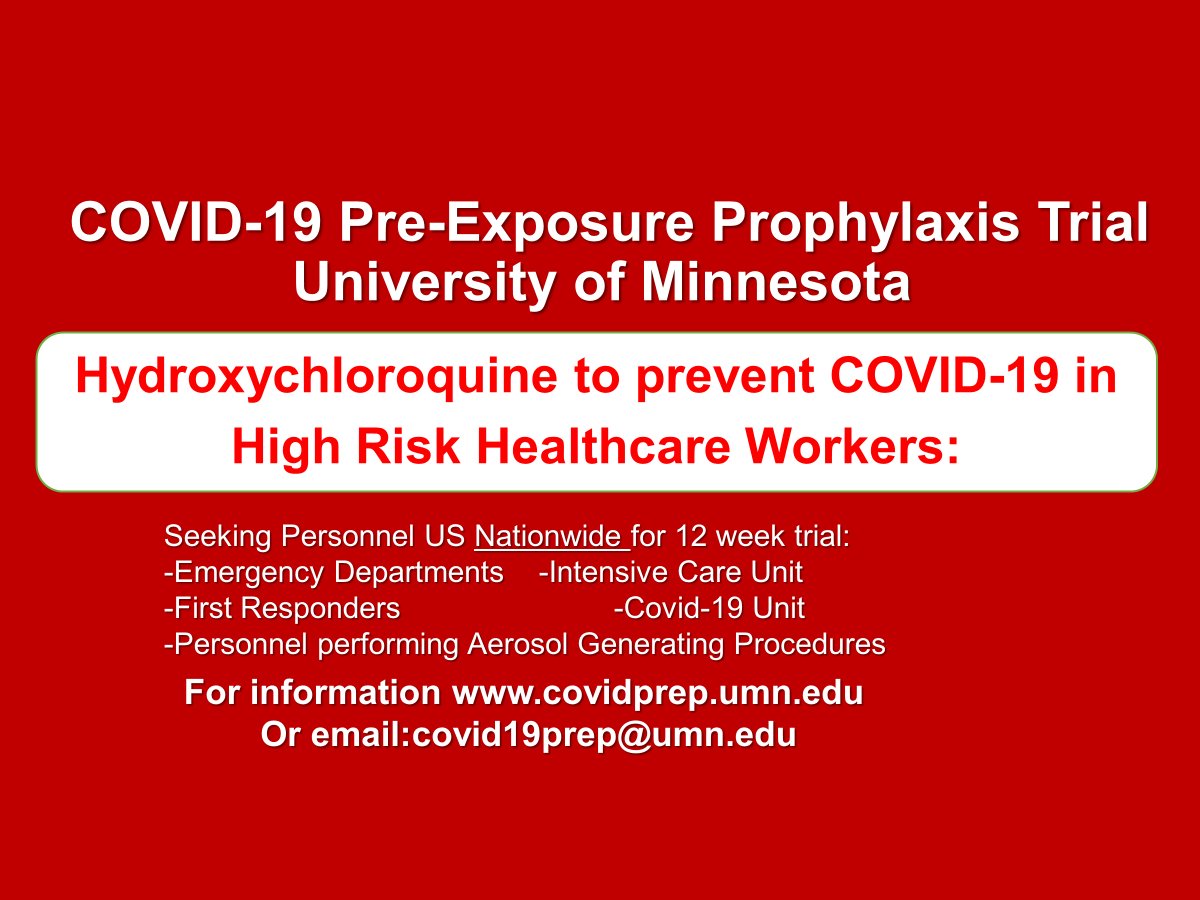
Though many people are pinning their hopes on a COVID-19 vaccine, another option is available: preventive treatment. At a Senate hearing this week, Anthony Fauci noted that a vaccine — which is probably months or years away — isn’t the only way to protect someone from a life-threatening virus.These treatments could protect people against infection for a few weeks or months, said Fauci, the director of the National Institute of Allergy and Infectious Diseases. While most ongoing research studies are focused on finding treatments for people who are already sick with COVID-19, some researchers are looking to see if they can stop people who are at high risk from getting sick in the first place.It’s a proven strategy: preventive drugs have been used for decades to help people protect themselves against malaria. More recently, they were a breakthrough in the fight against HIV. There’s no effective vaccine against HIV, but people can take a daily medication that reduces their risk of contracting it through sexual activity by 99 percent. The medication is a pre-exposure prophylactic, or PrEP — a drug used to prevent disease in people who haven’t yet been exposed to it.“We have an incredibly powerful tool that can, for myself personally, protect me from HIV,” says James Krellenstein, co-founder of the PrEP4All Collaboration and an organizer of a COVID-19 working group in New York.Krellenstein published a report this week outlining the clinical trials underway to find drugs that can prevent COVID-19. Viruses make people sick when they replicate and spread through the body, and most anti-viral drugs are designed to stop that replication process. Giving someone the drug early, when there’s only a small number of virus particles in the body, is going to be more effective than waiting until the virus is everywhere, Caleb Skipper, an infectious disease postdoctoral fellow at the University of Minnesota, told The Verge. In theory, a drug could be even more effective if it’s already in the body when the first virus appears.Skipper is part of a research team at the University of Minnesota running a clinical trial to see if hydroxychloroquine, which can stop the coronavirus from replicating in a test tube, can help keep health care workers from catching COVID-19. The drug has been the subject of a lot of controversy and hasn’t been able to effectively treat people who are already sick and hospitalized.Ongoing enrollment for Pre-exposure prophylaxis (PrEP) trial for high risk healthcare workers and first responders anywhere in the US (and parts of Canada soon). covidprep.umn.edu #MedTwitter




















1 comments:
Take on epic quests and claim your rewards Hawkplay
Post a Comment