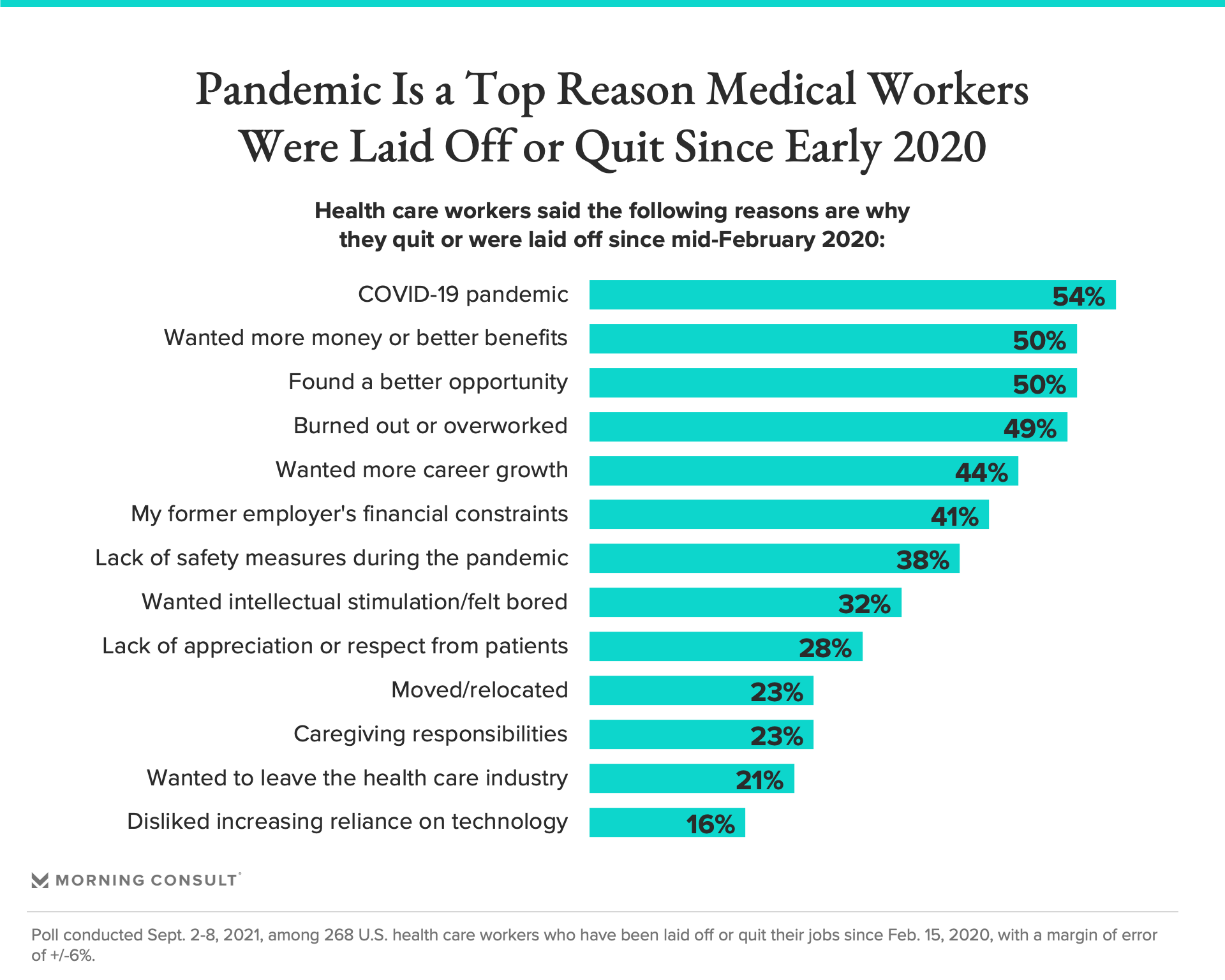
The top reasons for healthcare workers leaving were stress from the pandemic, compensation, burnout, found a better job, wanted more career growth. JL
Gaby Galvin reports in Morning Consult:
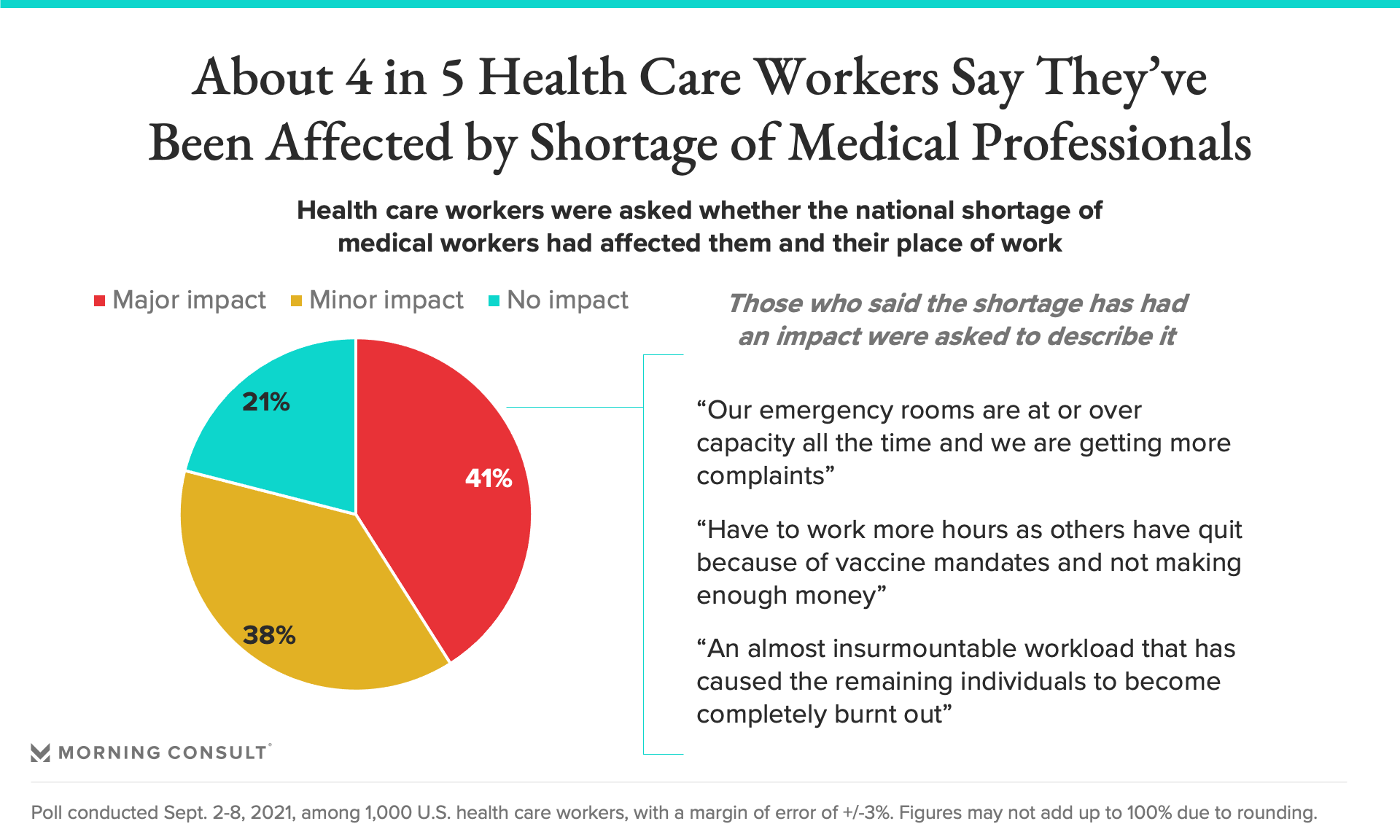
That exodus — driven largely by the pandemic, insufficient pay or opportunities and burnout, according to the survey — has implications for the entire health care system, both in the short term. 79% of health care workers said the national shortage of medical professionals has impacted them and their place of work. When asked to describe in an open-ended survey how they’d been affected by the shortages, many said their workloads had increased, sometimes leading to rushed or subpar care for patientsU.S. hospitals are filled with COVID-19 patients as the delta variant continues to ravage the country. Yet a year and a half into the pandemic, many health care providers are facing severe staffing shortages, and a new Morning Consult survey suggests more could be on the horizon.
In California, for example, thousands of Kaiser Permanente nurses said they’re planning a strike because of planned “hefty cuts” to their pay and benefits. In Michigan, Henry Ford Health System is turning to recruiting firms to bring 500 nurses from the Philippines to its hospitals over the next few years. And in upstate New York, a local hospital announced it would pause maternity services after dozens of staffers quit rather than get the COVID-19 vaccine.
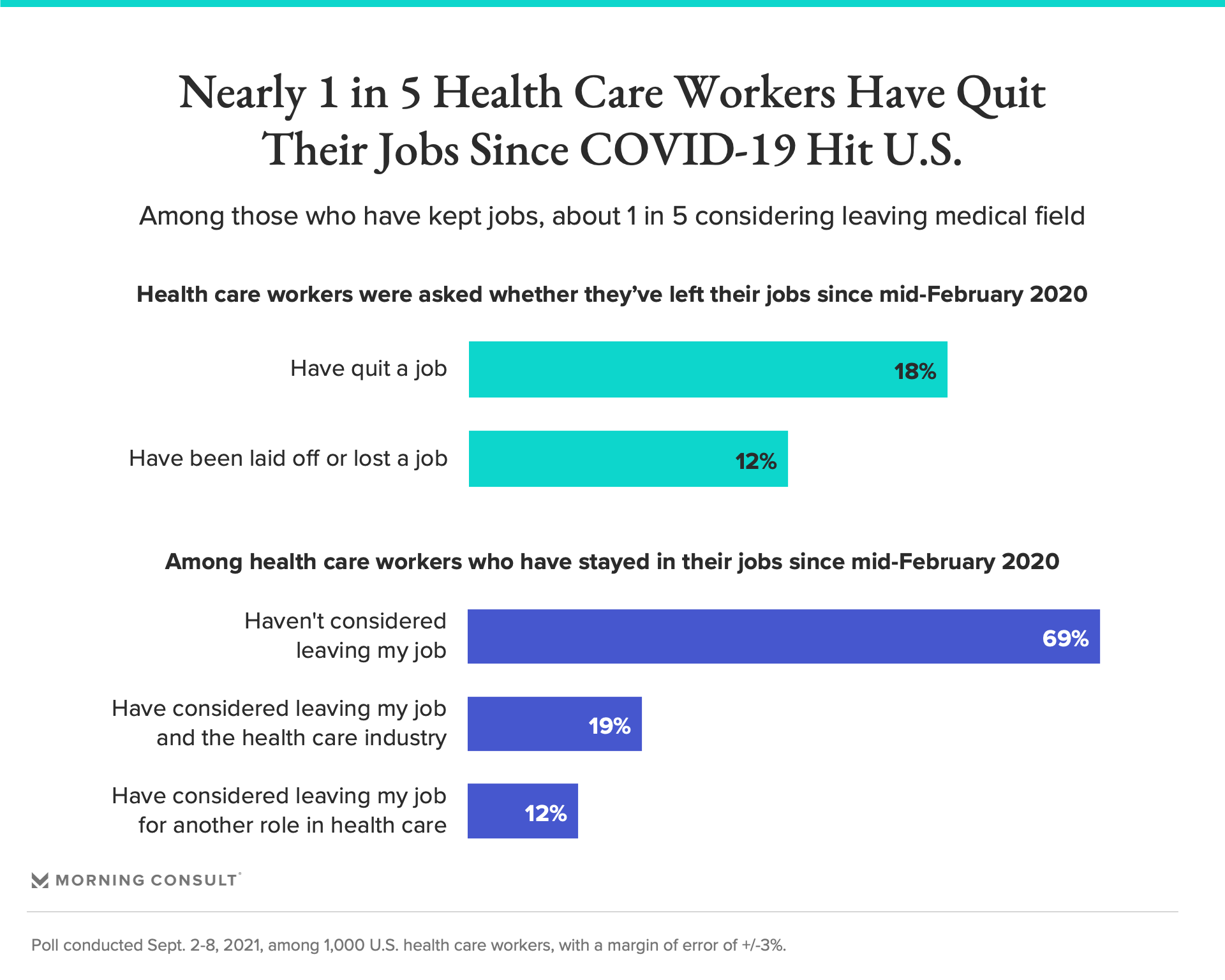
The survey indicates the medical staffing problems are widespread. It found that since February 2020, 30 percent of U.S. health care workers have either lost their jobs (12 percent) or quit (18 percent), while 31 percent of those who kept them have considered leaving their employers during the pandemic. That includes 19 percent who have thought about leaving the health care field entirely.
That exodus — driven largely by the pandemic, insufficient pay or opportunities and burnout, according to the survey — has implications for the entire health care system, both in the short term as the country struggles to overcome the COVID-19 pandemic and beyond as the country continues to age.
“You have physicians, you have nurses, dropping out, retiring early, leaving practice, changing jobs,” said Dr. Dharam Kaushik, a urologist at the University of Texas Health, San Antonio. “You’re experiencing loss of manpower in a field that was already short on manpower before the pandemic hit.”
In August, private health care employment was down by more than half a million jobs from February 2020, according to an analysis from Altarum. The job growth recovery has been slower for women than for men in 2021, as of May.
Hospitals and other providers have been “trying to stay afloat and care for patients” and leaning heavily on their clinicians and other staff to work overtime in taxing jobs, said April Kapu, associate dean for community and clinical partnerships at the Vanderbilt University School of Nursing and president of the American Association of Nurse Practitioners.
“That hasn’t diminished,” she added, and “there are huge environmental support factors that need to be in place in the hospital.”
Indeed, 79 percent of health care workers said the national shortage of medical professionals has impacted them and their place of work. When asked to describe in an open-ended survey how they’d been affected by the shortages, many said their workloads had increased, sometimes leading to rushed or subpar care for patients, while others said their colleagues had left because of COVID-19 vaccination requirements.
“Sometimes I find myself running a building completely to myself with 47 residents,” one health care worker wrote, while another added that “employees are stretched to the limits.”
National Nurses United, the country’s biggest nurses union, argues that the country actually does have enough registered nurses to meet patient needs, citing federal data from 2017 that projects that in 2030, there will be seven states with a registered nursing shortage and three states with surpluses of more than 20,000.
The underlying reason health facilities are having staffing problems, according to Deborah Burger, a registered nurse and the union’s president, is that clinicians are leaving because of poor pay, burnout and COVID-19 safety concerns.
In the survey, 77 percent of health care workers said they approve of how their employers have handled the pandemic. Morning Consult asked the 19 percent who said they disapprove of their employers to elaborate in an open-ended question, and many cited poor communication around changing safety protocols, inadequate personal protective equipment, low pay and a general sense of being disposable.
“When the first wave hit in 2020 my coworkers and I didn’t feel supported at all by my employer,” one health care worker wrote, adding that while 2021 has been better, “me and others feel like we have been used and abuse [sic] during Covid with no attempt at gratitude.”
Meanwhile, nurses are increasingly turning to “travel nursing” roles, earning significantly more than they do as hospital staffers, due in part to an influx of federal emergency funding that hospitals received to keep them afloat during the pandemic.
In the poll, health care workers cited broad employment issues as some of the top reasons why they left their jobs or were laid off during the pandemic: 50 percent said they were seeking better pay or benefits, while the same share said they found a better opportunity elsewhere and 44 percent cited a desire for more career growth.
Many also said they quit or were laid off because of the pandemic or because they were burned out or overworked. Notably, another 23 percent said they left because of their caregiving responsibilities.
“I think a lot of their concerns would have been dealt with if they had adequate staffing and support,” Burger said.



















0 comments:
Post a Comment